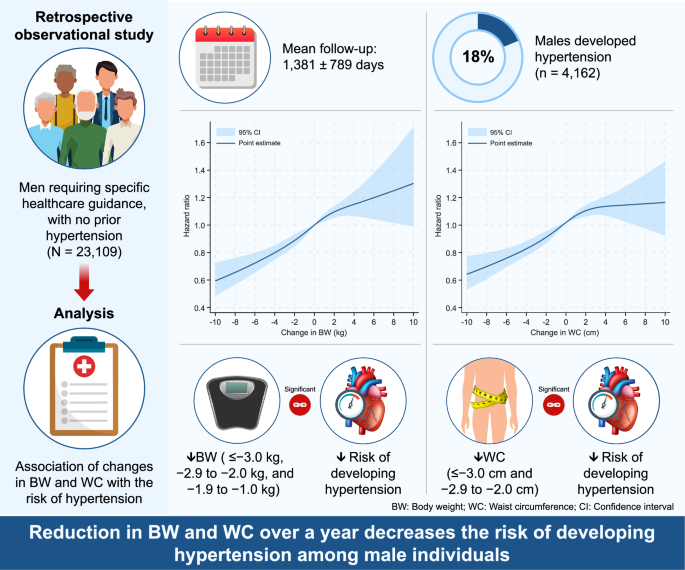
Study design
This study had a retrospective observational design and analyzed data from the DeSC database, which contains large-scale claims and medical check-up data between April 2014 and August 2023 provided by DeSC Healthcare (Tokyo, Japan) [7]. The DeSC database is a collection of annual health check-up records including data on blood pressure (BP) measurements, fasting blood examinations, medical history, current medications, and the individuals’ responses to a standard questionnaire of lifestyle habits. The DeSC database covers three major health insurance systems in Japan: the health insurance for employees of large companies (Kempo), the National Health Insurance for nonemployees (Kokuho), and the Advanced Elderly Medical Service System for older people aged ≥ 75 years (Koki Koreisha Iryo Seido). This broad coverage allows the DeSC database to be highly representative of the Japanese population across different age groups and socio-economic statuses. The comprehensive nature of the DeSC database strengthens the validity of our findings by ensuring a complete and more representative sample of the Japanese population. Annual health check-ups are mandatory for the general population in Japan, where more than 70% of men aged 45–54 years undergo health check-ups at least once a year [8].
There are two types of Specific Health Guidance in the fourth phase of the Specific Health Checkups and Specific Health Guidance program [1]. The intensive health guidance program is offered to those who have two or more risk factors with abdominal obesity or three or more risk factors with overweight (BMI ≥ 25 kg/m2) but without abdominal obesity. Abdominal obesity is defined as waist circumference ≥ 85 cm in men. The four risk factors are (1) hemoglobin A1c [HbA1c]≥5.6%, (2) triglycerides≥150 mg/dl and/or high-density lipoprotein cholesterol<40 mg/dl, (3) systolic blood pressure≥130 mmHg and/or diastolic blood pressure≥85 mmHg, (4) smoking status. Another program, referred to as the motivational health guidance program, is offered to individuals who have one risk factor with abdominal obesity or two risk factors with overweight without abdominal obesity. In this study, we focused on individuals classified as in need of specific healthcare guidance (active support in the intensive health guidance program) without a prior diagnosis of hypertension and without the use of blood pressure-lowering medications.
Ethics statement
The study was approved by the Ethics Committee of the University of Tokyo (approval number:2021010NI) and conducted in accordance with the Declaration of Helsinki. The requirement for informed consent was waived because all data included in the dataset were de-identified.
Study participants
We analyzed data for 30,374 men aged 40-64 years who were enrolled in the DeSC database between April 2014 and August 2023 and classified as in need of specific healthcare guidance (active support in the intensive health guidance program) without a prior diagnosis of hypertension and without blood pressure-lowering medications. Individuals with a history of cardiovascular disease (n = 280), with missing data on cigarette smoking (n = 35) and physical activity (n = 5924), with cardiovascular disease event within one year (n = 244), and with hypertension event within one year (n = 782) were excluded. Finally, we assessed the association of one-year change of BW and WC with the incidence of hypertension in 23,109 men (Fig. 1).
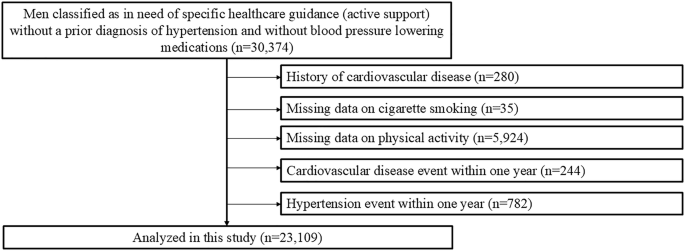
Flowchart. We identified 30,374 men classified as in need of specific healthcare guidance (active support) without a prior diagnosis of hypertension and without BP lowering medications in the DeSC database. We excluded individuals for the following reasons: a prior history of cardiovascular disease; missing data on cigarette smoking and physical activity; cardiovascular disease event within one year; and hypertension event within one year. Finally, we analyzed 23,109 participants
Measurements and definitions
We obtained the data of body mass index (BMI), WC, BP and laboratory data (HbA1c, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, and triglycerides). Information on history of smoking (current or non-current) and physical activity (active or inactive) was obtained from a self-reported questionnaire completed during the health check-up. Physical activity was defined as 30 min of exercise at least twice a week or ≥ 1 h of walking per day [9]. In the Japanese health check-up system, healthcare professionals measure the BP using a standard sphygmomanometer or an automated device at least twice after the participant has been in a resting condition, and the average is recorded [10, 11].
We defined diabetes as an HbA1c ≥ 6.5% or use of blood glucose-lowering medications and dyslipidemia as low-density lipoprotein cholesterol≥140 mg/dL, high-density lipoprotein cholesterol<40 mg/dL, triglycerides ≥ 150 mg/dL, or use of lipid-lowering medications.
Outcome
The primary outcome was incident hypertension (ICD-10 codes I10-I15) [12]. Study participants were followed until the incidence of the outcome, loss of insurance coverage, death, or study end date (August 2023).
Statistical analysis
Continuous variables were presented as the median (25–75th percentiles) and categorical variables as the number (percentage). We conducted multivariable Cox regression analyses to assess the association of changes in BW and WC with a subsequent risk of developing hypertension. Hazard ratios (HRs) and 95% confidence intervals (CIs) for developing hypertension were calculated for each value of change in BW using a BW change category (≤ −3.0 kg, −2.9 to −2.0 kg, −1.9 to −1.0 kg, −0.9 to 0.9 kg, 1.0 to 1.9 kg, 2.0 to 2.9 kg, 3.0 kg ≤) and for each value of change in WC using a WC change category (≤ −3.0 cm, −2.9 to −2.0 cm, −1.9 to −1.0 cm, −0.9 to 0.9 cm, 1.0 to 1.9 cm, 2.0 to 2.9 cm, 3.0 cm ≤) after adjustment for age, BMI, WC, systolic BP, diastolic BP, diabetes, dyslipidemia, smoking, and physical inactivity.
To validate the robustness of our primary findings, we examined the association of changes in BW and WC with a subsequent risk of developing hypertension using a restricted cubic spline regression model with four knots (5, 35, 65, and 95 percentiles). Hazard ratios were adjusted for age, BMI, WC, systolic BP, diastolic BP, diabetes, dyslipidemia, smoking, and physical inactivity.
In a sensitivity analysis, the outcome was redefined as a diagnosis of hypertension with a prescription for antihypertensive medications in the months before and after the diagnosis.
All analyses were performed using STATA version 19 (StataCorp LLC, College Station, TX, USA). A p-value < 0.05 was considered statistically significant.
link




