Principal findings
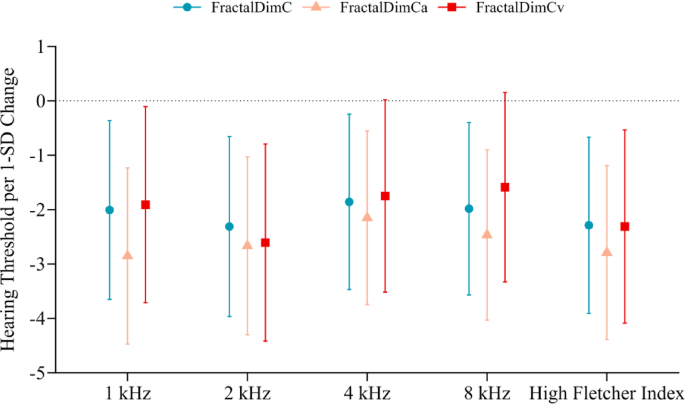
This cross-sectional study found a significant association between FD and HL in a health checkup population. Our results indicate that higher FDa, FDv, and total FD values were associated with better hearing acuity, as reflected by lower hearing thresholds. Specifically, each 1-SD increase in FDa and FDv was associated with a 2.85 dB HL reduction at 1 kHz and a 2.61 dB HL reduction at 2 kHz, respectively. These associations remained consistent across frequencies and with the hFI. Restricted cubic spline regression confirmed that the risk of hearing loss decreased as FD values increased. These findings suggest that retinal microvascular abnormalities could serve as systemic markers involved in the pathophysiology of HL.
Comparison with previous studies
Our findings support and expand previous research on the relationship between retinal microvascular abnormalities and HL. The Blue Mountains Hearing Study, the first international study to investigate this association, found a significant link between retinal microvascular abnormalities and HL, highlighting the importance of systemic microcirculation in hearing function23. Similarly, Kim et al., in the ARIC-NCS cohort, confirmed that retinal microvascular signs, such as retinopathy, were associated with hearing impairment, particularly among non-DM individuals24. Sardone et al. also identified an inverse relationship between retinal vascular density and central auditory processing disorders in older adults25. In contrast, our study uniquely used FD to comprehensively measure vascular complexity, providing a broader evaluation of retinal microvascular health and its relationship with HL across various frequencies. This approach suggests that FD may be a more sensitive marker for detecting systemic vascular changes related to HL.
Biological or clinical mechanisms
The association between FD and HL observed in this study may be due to shared microvascular pathologies affecting retinal and cochlear circulation. Since retinal and cochlear tissues are highly vascularized and sensitive to ischemic damage, they are vulnerable to systemic microvascular dysfunction31,32. Reduced retinal vascular density may indicate underlying microvascular insufficiencies affecting cochlear blood flow, leading to sensory hair cell degeneration and subsequent HL23,24. An example supporting this association is Susac syndrome, a rare condition involving occlusive microvascular disease of the brain, retina, and inner ear, which demonstrates how microvascular pathology can impact both retinal and auditory structures23,33.
Another possible cause is endothelial dysfunction in microcirculatory networks, as endothelial cells play an important role in vascular tone modulation and blood flow dynamics34. Malfunctions in these cells can undermine the blood-labyrinth barrier in the cochlea, which is crucial for preserving the electrochemical equilibrium necessary for auditory function35. The disruption of this barrier could hinder the ion transport mechanisms regulated by the stria vascularis, resulting in auditory dysfunction35.
Furthermore, the FD of retinal vessels provides an integrated measure of vascular complexity and efficiency by quantifying the scale-invariant branching patterns of the retinal vascular network, encompassing characteristics such as bifurcation frequency, branch angles, and segment lengths26,36. A lower FD indicates a simplified vascular architecture with reduced branching density26potentially compromising tissue perfusion in the retina and cochlea. Notably, lower FD and density are associated with increased risks of mortality, cardiovascular diseases, DM, sleep apnea, and anemia26,37. Therefore, reduced retinal FD may serve as a marker of generalized vascular aging or early microvascular disease, linking systemic vascular health to sensory impairments like HL23,24.
In addition to the hypotheses previously discussed, we propose two additional testable mechanisms that may explain the observed association between reduced retinal vascular FD and HL.
First, a deficit in neurovascular coupling: recent findings from brain studies indicate that pericytes along capillary walls actively regulate vessel tone and local blood flow in response to neuronal activity38. Loss or dysfunction of these pericytes can impair neurovascular coupling and reduce oxygen delivery. A similar mechanism may exist in the cochlea, where pericytes are densely distributed in the stria vascularis and spiral ligament, contributing to the regulation of cochlear blood flow15. Disruption of pericyte-mediated regulation in the cochlear microvasculature may result in transient ischemia, potentially accelerating HL.
Second, a deficit in glymphatic-like clearance: the cochlea has been reported to contain a glymphatic-like system that removes metabolic waste (e.g., amyloid-β) via paravascular fluid transport, similar to the brain’s glymphatic pathway39. As indicated by lower retinal FD, a reduction in systemic microvascular complexity may compromise this clearance mechanism, leading to toxin accumulation and damage to auditory structures. These mechanisms provide biologically plausible links between retinal and cochlear microvascular health and warrant further investigation in longitudinal studies.
Strengths and limitations
To our knowledge, this is the first study using FD as a metric to examine the relationship between retinal vascular characteristics and hearing loss across low and high frequencies. FD provides a broader evaluation of retinal microvascular health, capturing the overall complexity of vascular branching patterns, which traditional metrics such as CRAE, CRVE, and AVR, primarily focused on vessel diameter, may fail to capture adequately36. Previous studies have shown that lower FD and density are significantly associated with increased risks of mortality, hypertension, stroke, congestive heart failure, renal failure, DM, sleep apnea, and anemia26,38. By analyzing FD, we captured broader patterns of vascular complexity that may play a role in the pathophysiology of HL. These patterns might be overlooked when examining only specific vessel calibers. Additionally, the relatively large sample size from a routine health checkup population improves the generalizability of our findings, supporting their relevance in non-clinical settings. Another strength is the rigorous statistical adjustment for potential confounders, including age, sex, smoking, alcohol consumption, and chronic conditions such as hypertension, coronary heart disease, DM, and HYP, which enhances the robustness of our results.
This study has several limitations. Firstly, the cross-sectional design restricts our ability to establish causal relationships between retinal vascular changes and ARHL, leaving it uncertain whether these microvascular alterations precede or follow hearing loss. Longitudinal studies are needed to clarify this temporal association. Secondly, residual confounding variables such as nutrition, physical activity, and medication usage may persist despite adjustments for major confounders. Thirdly, the absence of bone conduction audiometry limits our capacity to differentiate between sensorineural and conductive HL. Lastly, although the observed effect sizes were small, even modest associations may hold clinical relevance at the population level.
Future directions
This study highlights the association between FD and HL, although further investigation is needed. Longitudinal studies are critical to establish causation and determine whether retinal microvascular changes occur before HL. Second, future studies should incorporate bone conduction audiometry to distinguish between sensorineural and conductive HL. Third, exploring the management of systemic conditions such as hypertension and diabetes and their effects on HL is valuable, as is investigating lifestyle factors such as diet and physical activity40,41. Finally, advanced imaging techniques such as optical coherence tomography angiography could offer more precise retinal vascular assessments and a more detailed understanding of microvascular changes associated with HL42.
link