Participant characteristics
Nineteen individual interviews were conducted in the HCP and scientist cohort, comprising Clinicians (n = 7), Scientists (n = 10) and Clinician/Scientists (n = 2). Practice areas included Genetic counseling, Pediatrics, General practice, Aboriginal health, Metabolic, Respiratory, Immunology, Pediatric Hematology, Clinical Genetics, Genetic Pathology, and Neurology. Twelve interviews (10 individual interviews and two small group discussions) were conducted with 16 policy-makers across NBS, genomics, or HTA. Participants were located around Australasia, with a minimum of two per jurisdiction (Table 2).
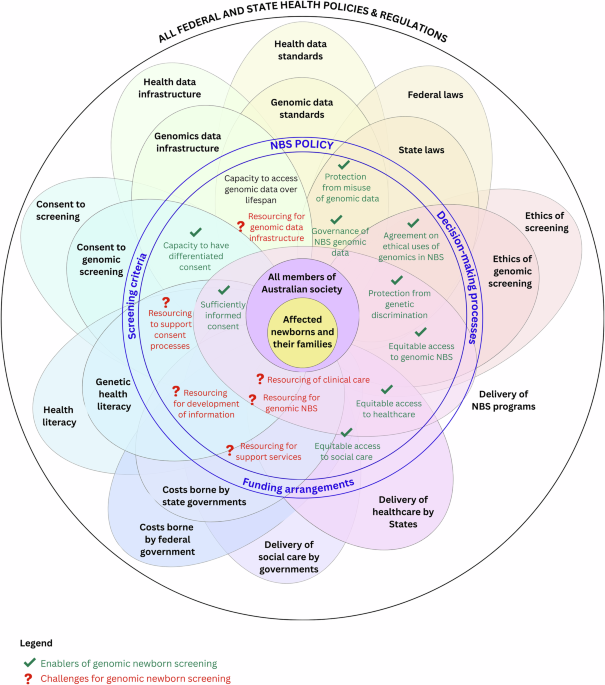
Participants’ views on potential benefits and risks of using genomics in NBS
While HCPs, scientists and policy-makers acknowledged the potential benefits of genomics in NBS, risks were more frequently identified (Table 3). Participants emphasized that the health system is not yet equipped to accommodate genomic NBS safely and effectively. While acknowledging lack of readiness, a small number of participants in each cohort felt that genomic NBS was imminent, and that it may be best for Australia’s governments and health system to be prepared. For those participants there was a fear that Australia’s health system is not ready for genomic NBS.
“It’s not a matter of if, but a matter of when, basically. And, for me, that’s slightly scary because it’s almost like we are jumping a bit too far ahead of ourselves”. [Clinician/Scientist #18]
Participants across all cohorts highlighted evidence gaps needed for government decision-making on genomic NBS, particularly around treatment safety, clinical and cost-effectiveness for rare conditions, and the penetrance and genotype–phenotype associations of certain variants.
“But there’s a lack of evidence and data to help us make those policy decisions, because things are moving so fast in genomics.” [Policy-maker #12]
Some policy-makers raised concerns about public attitudes toward genomics, questioning whether families would want to know their child’s genetic information, particularly for conditions that are not immediately medically actionable. They stressed the importance of implementing genomic NBS in a cautious, ethical and safe manner, rather than being driven by technology.
“The technology is there…and the research agenda is significant but we are a long way from being ready at a high level.” [Policy-maker #9]
Almost all participants pointed to the complexity for government policy of balancing a population health approach to screening with the individual needs and preferences of families. While the potential for genomics to reduce infant morbidity and mortality in population screening was acknowledged, participants felt that benefit must be carefully balanced with harm at a population level.
“…on balance, you would want to ensure that the benefit far outweighs the harm.” [Scientist #7]
Several HCPs raised concerns about the low sensitivity of genomic newborn screening to detect genetic variants for individuals of non-Caucasian ancestry due to the under-representation of diverse populations in current reference databases. One HCP noted that this may result in variants that are (mis)classified as variants of unknown significance (VUS) and not reported. This was seen as a source of potential inequity, particularly for Indigenous Australians and smaller populations, who may be at greater risk of false negatives or uncertain results. While some acknowledged ongoing efforts to build more inclusive genomic datasets, others noted the limitations of achieving true equity given small and genetically diverse population sizes.
“…[t]here might be certain populations where you do get a result…and you’d get all these variants of unknown significance, because there’s not enough data and not enough evidence and research to tell us whether that’s actually a negative result or not.”
One scientist expressed hope that biochemical and genomic newborn screening could eventually be combined, using a multiomics approach to help resolve DNA-only variants of uncertain significance, but emphasized that such variants should not be reported in the meantime.
Defining use of genomics in NBS
Although participants distinguished between genetics (targeted sequencing of specific genes) and genomics (mostly referring to WGS), these terms were often used interchangeably. Views on whether WGS should be used in NBS were mixed without consensus, however many preferred the use of a targeted panel of genes, rather than WGS. Whether WGS data should be collected and retained by a laboratory as a lifetime data resource for the infant, or whether it should only be collected and reported to the child’s parents, was frequently raised. While some saw value in WGS for its potential to improve time to diagnosis, guide treatment decisions, and support reproductive decision-making, others thought that implementation should be guided by established screening principles.
Suitability of current NBS assessment criteria to accommodate genomics
It was acknowledged by some HCPs and scientists that using genomics in a population screening setting, rather than being an expansion of the current NBS program, would be a ‘paradigm shift’ (Table 4). Some policy-makers noted that genomics doesn’t fit ‘neatly’ into the health system and is often seen as a highly specialized area more often considered in the context of diagnosis than screening. Given its capacity to identify genetic variants for later onset conditions, or extend benefit beyond the newborn via carrier screening, some participants believed that the introduction of genomics to NBS requires a review of current screening criteria [6]. They believed that benefits to the newborn or the family should be considered. Others felt the existing criteria should remain unchanged, arguing that technology should be a secondary consideration, with NBS remaining focused on actionable conditions with a direct treatment-related benefit to the newborn.
Considerations for NBS program delivery
National consistency in NBS delivery across Australian jurisdictions was seen by all participants as a key enabler for genomic NBS. Developing strict, yet flexible, national screening and reporting criteria was seen as critical to the introduction of genomic NBS to avoid geographic differences in screening.
“…if we’ve got all of these conditions that are screened for, they need to be the same around Australia.” [Scientist #2]
Some HCPs and scientists acknowledged this may not be achieved across all jurisdictions initially but felt that this should not stop implementation. Policy-makers suggested that equity in program delivery across jurisdictions could vary, with differing levels of capacity to implement genomic NBS across states and territories.
“A national approach…is potentially an enabler rather than a disadvantage because…there’s less inequity depending on cost and access and those things.” [Policy-maker #9].
A national approach to consent was viewed necessary for successful implementation of genomic NBS. Participants consistently identified consent as a major challenge, alongside ethical and equity concerns. Most commented that the current model of consent for Australia’s NBS program is based on inferred, rather than informed, consent with many noting that parents whose children undergo the NBS heel prick test often have poor recall of giving consent. Participants felt that, with genomics potentially introducing increased uncertainty and complexity in screening results compared to the current NBS program, parents may require additional support and counseling to understand the potential consequences of their child undergoing genomic NBS.
“…when we think about what consent should look like, it’s balancing up…how much information do people need to know and how much do they want to know?” [Clinician/Scientist #19]
Given the challenges experienced by parents and families during the newborn period, many participants suggested that consent for genomic NBS should occur during pregnancy (ideally later in pregnancy), with a follow-up conversation at birth. Some also saw consent as an opportunity for public education on genomics to ensure parents have a clear understanding of screening and diagnostic processes. However, a small number of HCPs and scientists questioned the feasibility of achieving fully informed consent at a population level.
“There’s no way you can get 300,000 people a year informed consent. All you can do is provide good quality accessible information in as many languages as possible. Leave it at that.” [Scientist #14]
Health workforce and system capacity to accommodate genomic NBS
Insufficient health workforce was consistently identified as a critical barrier to genomic NBS. The anticipated increase in the number of conditions detected through genomic NBS, along with enhanced monitoring and surveillance, was highlighted as a key challenge due to the potential for uncertain genotype-phenotype associations and the identification of more asymptomatic conditions.
“We don’t have the workforce, we don’t have the infrastructure. So there’s also very practical nut and bolt type things to be worked through.” [Scientist #7]
It was identified that more genetic counsellors are needed, and their scope of practice may need to evolve to include obtaining consent and supporting families receiving a positive or uncertain screen result or a genetic condition diagnosis. HCPs regularly identified genomics literacy of the health workforce as an area requiring attention if genomic NBS were to be introduced.
“…our hospital is building up a genetic counsellor network to help with explaining the genetics…You don’t want somebody who’s never seen a case of something explaining it to new parents.” [Clinician/Scientist #19]
Some HCPs and scientists emphasized that health service planning for genomic NBS cannot stop at diagnosis and requires a culturally-sensitive model of care which supports the newborn and family through diagnosis and treatment. Some pointed out that the conditions detected by genomic NBS should still be rare and did not see genomic NBS as being different from current NBS in terms of access to treatment and specialist care for those in rural and remote areas.
“…you’d potentially be sticking thousands of results into the healthcare system, without having had the chance to build up the capacity”. [Clinician/Scientist Interview #4]
A small number of policy-makers also identified equity implications at the health system and state and territory level, for example, differences in reference ranges for conditions, treatment and care pathways, approaches to data collection, storage and use, and capacity to implement genomic NBS.
Laboratory and data infrastructure
The capacity and coordination of laboratory testing infrastructure were identified as both a current barrier and a key enabler for the implementation of genomic NBS. Policy-makers emphasized the importance of adopting a national approach to laboratory infrastructure to ensure consistent delivery of genomic NBS across jurisdictions. HCPs and scientists generally supported a nationally coordinated, well-funded lab system, but differed on whether to centralize genomic NBS at one site or integrate it into existing labs nationwide. A few HCPs and scientists noted that the integration of biochemical and molecular screening services is important for effective implementation of genomic NBS. Participants highlighted a lack of workforce experience and capacity in genomic screening and diagnostics within Australia, with demands exacerbated by the introduction of genomics to NBS.
“…we’re struggling to deliver diagnostic genomic testing now, and the growth of the workforce and capacity to deliver genomics in Australia is not really there.” [Clinician/Scientist #4]
Although it did not emerge as a dominant category, one scientist and a small number of policy makers commented on the capacity of laboratories to report results within an acceptable timeframe for genomic NBS, particularly for those conditions which require identification within the first few days after birth. All participants acknowledged the large volume of data that genomic NBS could generate if WGS was implemented, including information that may not be directly relevant for diagnosis or clinical care.
“There are people who think that having the whole genome would be great, and that we could re-analyze it across the lifetime. But…it comes with issues of cost of storage and privacy, and how do you keep that information secure?” [Policy-maker #8]
The infrastructure and financial resources required to support data storage, privacy, security, and analysis were frequently cited as challenges for genomic NBS implementation. A small number of HCPs and scientists raised concerns about the secondary use of data, particularly by police and forensic agencies, which some participants felt would need to be carefully communicated to the public.
“…you’re generating all this genomic data that, under current rules, you have to keep. And there may be benefits to keeping it in terms of reanalysis later on…but you’re going to have the police knocking on your door on a regular basis once you’ve started.” [Scientist #14]
Genomic NBS costs and cost-effectiveness
All cohorts consistently identified the direct costs of genomic testing and the long-term cost-effectiveness of genomic NBS as key challenges. They noted tension between the benefits of detecting and treating more individually rare genetic conditions against low population incidence and higher costs for screening, data storage and analysis, and follow-up healthcare. While most participants acknowledged that the current cost of genomics was prohibitively high for widespread implementation in a universal screening program, some noted that these costs were expected to decrease over time.
“…the principles of when one should be using it should be exactly the same as the principles of any other technology…there has to be a demonstrable benefit and it has to be safe, and from a population perspective it has to be cost-effective.” [Policy-maker #8]
There was a shared belief by all participants that genomic NBS should be government-funded to ensure equitable access. Some thought that genomic NBS could be cost-effective for the health system by aiding earlier detection and prevention of serious illness. Others raised concerns about the potential for increased costs due to increased use of therapies for additional genetic conditions, and increased monitoring of presymptomatic newborns and those with an uncertain genotype-phenotype relationship.
“Unfortunately there’s a cost benefit ratio because obviously it comes down to cost in the end. Gene therapies are running into millions of dollars, so how many can we afford to do?” [Clinician #5]
link





