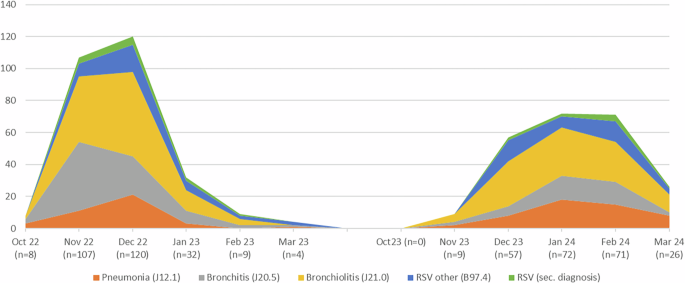
This study underscores the significant burden of RSV on healthcare systems, characterized by high rates of hospitalization and intensive care admissions. Our findings reveal notable parental hesitancy toward immunization primarily driven by knowledge gaps, concerns about safety / lack of trust and feelings of being rushed due to the timing shortly after birth. Our seasonal RSV data aligns with findings from cross-sectional studies from the U.S. [1, 2] and Germany [3, 4] underscoring the representativeness of our surveyed community.
While in the Netherlands, RSV-related PICU admission costs approximately 3.1–3.8 million € per season [9] for Germany Poshtiban et al. estimated the annual RSV-related health burden for the inpatient treatment of the pediatric population to be 66 million € [10]. These figures highlight the immense financial strain RSV places on healthcare systems, further reinforcing the importance of preventive strategies like immunization to reduce both clinical and economic burdens. As a consequence, the state of Bavaria has made efforts to sufficiently allocate its pediatric care resources via telecommunication [11] in order to maintain pediatric (intensive) care for non-infectious patients during RSV season [12].
Opportunities to enhance parental acceptance of RSV immunization: lessons from Bavarian and U.S. surveys
Our survey included 87 parents from two tertiary NICU centers, making it significantly larger than the contemporaneous study by Hinderstein et al. in the United States, which encompassed 28 interviews at a single center [13]. Notably, their study employed a different methodological approach. Utilizing the Health Beliefs Model as a conceptual framework, their study identified actionable opportunities to influence perception-based factors such as susceptibility, severity, benefits, and barriers, as well as decision-making drivers like self-efficacy and cues to action. Consistent with our findings, Hinderstein et al. [13] demonstrated that parental acceptance of nirsevimab remains a critical challenge despite its official approval, partly shaped by negative perceptions linked to prior experiences with the COVID-19 vaccine and the miscommunication surrounding its rollout [14]. Additionally, they identified persistent barriers such as knowledge gaps, misinformation, and concerns about safety, with key issues including confusion between monoclonal antibodies and vaccines, as well as the influence of provider trust [13]. Noteworthy, trust in clinicians has long been recognized as a critical factor influencing vaccine decision-making and remains a highly influential determinant [15], however, the limited time available during the short stay after birth makes it challenging for pediatricians to establish a strong and healthy foundation of trust. In our study, parental acceptance of RSV immunization may have been positively influenced by providing sufficient information in advance and allowing more time for consideration, emphasizing the need to shift vaccination-related discussions earlier in the care continuum. This emphasizes the importance of implementing robust prenatal information campaigns addressing these barriers, particularly through obstetricians, to ensure parents are adequately informed before delivery.
While nearly 80% of parents in our study reported being informed about the impact of RSV in general, we did not assess the accuracy or depth of their knowledge, which represents a limitation of our study. However, rejection of immunization in our cohort was often linked to a clear knowledge gap and fears about potential side effects. Hinderstein et al. similarly found that some parents perceived nirsevimab as “new and understudied,” emphasizing the critical need for transparent communication about its safety profile, its similarity to established antibodies, and its rigorous clinical evaluation [13].
Such efforts would help to unlock the true potential of this intervention by reaching more children. This aligns with the groundbreaking potential of RSV immunization to transform pediatric intensive care by significantly reducing RSV-related hospital and NICU admissions.
Leveraging media to build trust and combat misinformation
In times where parents commonly seek health-related information online, social media can positively influence vaccination-related behaviors during pregnancy. Unfortunately, it may also serve as a platform for spreading misinformation [16]. In this context, our recent analysis of German health information available online highlighted the diminished quality of content, partly driven by the growing trend of commercializing information [17]. In addition, recent efforts to maintain fact-checking on online platforms are being scaled back, even though our survey and the study by Hinderstein et al. [13] show that these platforms remain important sources of information for (future-to-be) parents and tools to counter potential misinformation [18]. Medical societies are uniquely positioned to leverage these media channels to disseminate accurate information, counter misinformation, and build trust by engaging a broad audience with authoritative and evidence-based guidance.
The role of public health in shaping perceptions
Considering the safety aspects and in the international context, professional societies such as the German Society for Gynecology and Obstetrics (DGGG) support the recommendation to administer the maternal RSV vaccine from 32 to 36 weeks of pregnancy [19,20,21,22]. Currently, however, the maternal vaccine is not yet listed in the German Vaccination Guideline and is therefore not covered by general health insurance and reimbursement for private patients is not possible.
At the time of writing this article, the structural requirements (economic, insurance and medical personnel) to implement the newborn immunization program comprehensively were under discussion with the Federal Ministry of Health in Germany and carried out in public [23,24,25]. At this time, the Association of Leading Pediatric and Adolescent Doctors in Germany (VLKKD) has estimated the need for a 25% part-time job for the immunization of 1000 births in the period from October to March, with an investment of €300-350,000 for the vaccine and approximately 20 min per immunization including informative conversation, patient consent and documentation [26].
link






